A fracture of the cervical vertebrae is similar to any other fracture in the body, except that the consequences can be more serious if not treated in a timely fashion. When the spine is fractured, portions of the vertebrae can begin to irritate the spinal nerves and cause localized or radiating pain. In more serious cases, the vertebrae can enter the spinal canal and result in far more serious symptoms. It is important to know how cervical fractures occur and what effective treatment options are available.
Common Causes
Any abrupt impacts that causes whiplash—the jolting of the neck back and then forward—can result in a cervical vertebrae fracture. The most common types of fracture resulting impact situations are:
- A motor vehicle accident (MVA)
- A head-on collision while playing sports
- A sudden blow to the head
In addition to fracturing one (or more) of the cervical vertebrae, whiplash can cause the ligaments of the cervical spine to stretch, partially tear, or rupture. This can lead to instability of the cervical spine that affects the spinal cord as well as motor functions.
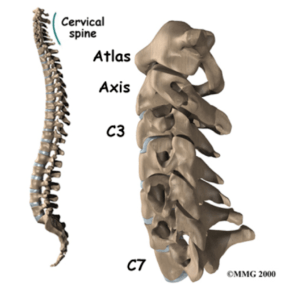
Illustration 1- The seven cervical vertebrae of the spine
Non-Surgical Treatments
Non-severe cervical fractures can often be treated non-surgically. Common treatments include:
- Cervical braces help temporarily immobilize the neck so the fracture can heal.
- Pain medication. Moderate to severe pain following a whiplash injury is common. Non-narcotic and narcotic medications may be given to help reduce pain.
It’s important to note that in most cases a combination of any or all of the above treatment options may be used.
Surgical Treatments
In more severe cases, cervical fractures are classified as “unstable”, which means that they will not heal properly without a surgical intervention. The goal of surgery is to reduce the fracture, stabilize the bone (usually via fusion), and, if need be, restore neurological and motor function.
The three most common types of surgery are:
- Minimally Invasive Posterior Cervical Fusion
- Minimally Invasive Anterior Cervical Decompression and Fusion
- Minimally Invasive Cervical Spinal Fusion
The type of procedure that’s performed is based on the patient’s injury and the decision of the neurosurgeon.
Role of the Neurosurgeon
If you or someone you know sustains a significant cervical spine impact, diagnosing the severity of the injury is the top priority. In most cases, going to the emergency room is the first step. Once the injury has been properly X-Rayed, you will most likely be told to follow up with a neurosurgeon. The neurosurgeon’s diagnosis and treatment plan will help stabilize the fracture and avoid any permanent damage to the spine. A full recovery and return to normal function are almost always possible.
Dr. Patrick Senatus is a Board Certified Neurosurgeon in New York City with extensive experience in Minimally Invasive and Restorative Spine Surgery. Dr. Senatus attended Harvard College where he was recognized as a Harvard College and John Harvard Scholar and graduated Magna Cum Laude with a Bachelor of Art in Biochemical Sciences. As a medical scientist training program scholar he completed his Doctorate of Medicine at Harvard Medical School and his Doctorate of Philosophy in Neurobiology at the Harvard Graduate School of Arts and Sciences.
In 2006, Dr. Senatus completed Neurosurgery Residency at Columbia Presbyterian Medical Center where he was nominated for the Arnold P. Gold and Physician of the Year Award, recognizing him for excellence in teaching and patient care. Subsequently, he completed a fellowship at the Cleveland Clinic in Functional and Restorative Neurosurgery of the Spine and Brain.
If you, or someone you love, is suffering from chronic back or neck pain contact us today!

Recent Comments