Bone spurs, also known as osteophytes, are the bony outgrowths that can develop on the edges of the vertebrae due to the aging process or wear and tear. Bone spurs are most common in those over 60 years and older, but they do not always result in back or neck pain. In most cases, bone spurs are not painful by themselves and cause pain when they begin to irritate the spinal nerves, or rub against each other, which can then cause pain and other symptoms.
The lumbar spine is more prone to the formation of bone spurs as this area is typically subjected to more stress on a day-to-day basis. Bone spurs in the cervical spine are often the result of a previous injury or trauma to the cervical spine.
Causes of Osteophytes in the Spine
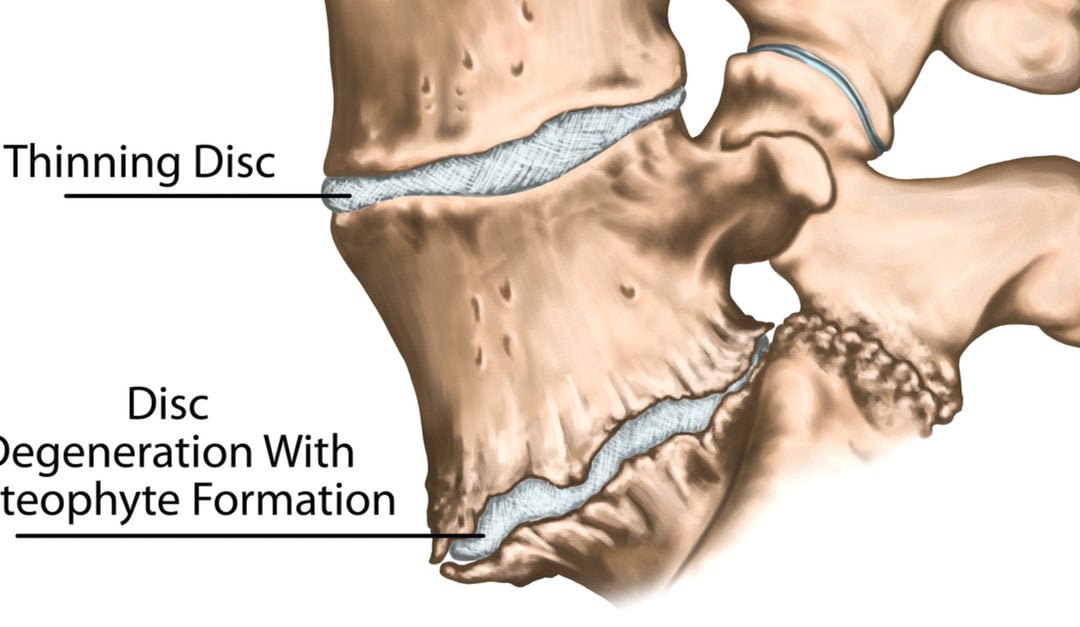
Spinal Disc Degeneration
Between each vertebrae in the spine are the intervertebral spinal discs which act as shock absorbers and prevent the vertebrae above and below from coming into contact. Over time, these discs can begin to degenerate or weaken due to repetitive trauma or simply just the aging process. As the discs become deteriorated the space between the vertebrae is reduced and can cause increased bone on bone contact. Also, as the disc degenerates the ligaments of the spine may begin to loosen and cause excess motion in the spinal joints, which can also increase bone on bone contact.
Osteoarthritis
Osteoarthritis is a process which breaks down the cartilage at the end of the bones. Once the cartilage is destroyed, the bones may rub against each other, leading to excessive wear and tear of the spine and result in the formation of bone spurs. Research shows that adults who are 50 and older will almost always develop some amount of degeneration of the lumbar spine. Life factors such as previous spinal injuries, excessive weight, arthritis in other joints and poor posture can increase the amount of degeneration.
DISH
DISH or “diffuse idiopathic skeletal hyperostosis” is a disease process that results in the hardening or calcification of the ligaments attached to the spine. As a result, large bone spurs develop on the spine.
Treating Osteophytes of the Spine
As mentioned above, the mere presence of spinal osteophytes doesn’t mean that treatment is needed. It is only when these osteophytes cause symptoms such as localized or radiating pain that treatment should be sought. It is important to consult a spine specialist at the first sign of symptoms so that the proper care path can be determined.
Physical Therapy
Physical Therapy is often the first course of treatment and many patients will experience continuous relief of pain after several weeks of Physical Therapy. The goal of Physical Therapy will be to strengthen the muscles that surround the spine, as well as the core muscles, to improve posture and help you avoid the positions that lead to painful episodes.
Injection Therapy
Injections such as anti-inflammatory or corticosteroids are often used either in conjunction with Physical Therapy, or if Physical Therapy has not provided adequate relief from pain. These therapeutic injections are administered under fluoroscopic guidance directly into the spinal nerve that is compressed or irritated by the spinal osteophyte. The goal of these injections is to reduce the inflammation that is causing pain and calm the irritated spinal nerve.
Minimally Invasive Procedures
In instances where Physical Therapy and injections have not provided consistent pain relief, a Minimally Invasive Surgical Procedure may be recommended to decompress the spinal nerve, or stabilize the spine.
The most common procedure utilized for osteophytes of the spine is known as a Minimally Invasive Laminectomy. During this procedure, a small incision is made over the affected level of the spine so that small instruments can be inserted. Next, the arched piece of bone at the back of the vertebrae, known as the lamina, is trimmed so that the spinal nerve root can be decompressed and will have more room in the spinal canal. If other bone spurs exist on the outside end of the vertebrae, known as the foramina, these may be trimmed or removed as well.
The incision is the closed with small sutures and a bandage. In most cases, patients are able to return home the same day as their procedure.
Dr. Patrick Senatus is a Board Certified Neurosurgeon in New York City with extensive experience in Minimally Invasive and Restorative Spine Surgery. Dr. Senatus attended Harvard College where he was recognized as a Harvard College and John Harvard Scholar and graduated Magna Cum Laude with a Bachelor of Art in Biochemical Sciences. As a medical scientist training program scholar he completed his Doctorate of Medicine at Harvard Medical School and his Doctorate of Philosophy in Neurobiology at the Harvard Graduate School of Arts and Sciences.
In 2006, Dr. Senatus completed Neurosurgery Residency at Columbia Presbyterian Medical Center where he was nominated for the Arnold P. Gold and Physician of the Year Award, recognizing him for excellence in teaching and patient care. Subsequently, he completed a fellowship at the Cleveland Clinic in Functional and Restorative Neurosurgery of the Spine and Brain.
If you, or someone you love, is suffering from chronic back or neck pain contact us today!

Recent Comments